Morphia Derma Understanding Its Role in Dermatology
Morphia derma, or morphea, is a rare skin disorder characterized by localized thickening and hardening of the skin. It is a form of scleroderma, which primarily affects the skin but may also involve underlying tissues. Understanding morphia derma involves examining its causes, symptoms, diagnostic methods, treatments, and potential complications.
What Is Morphia Derma?
Morphia derma is a form of localized scleroderma that leads to the formation of patches of thickened, discolored skin. The skin appears shiny, and hardened and may show areas of discoloration ranging from light to dark. Unlike systemic sclerosis, another type of scleroderma, the condition typically affects only the skin and does not impact internal organs.
Types of Morphia Derma
Plaque Morphia:
The most common form is characterized by one or more thick, oval patches of hardened skin.
Linear Morphia:
This type involves a linear band of thickened skin that can follow the lines of the body, sometimes affecting deeper tissues such as muscles or bones.
Generalized Morphia:
This rare form results in widespread skin thickening and can potentially cause significant physical limitations.
Pansclerotic Morphia:
It is a severe form where the skin thickens so much that it can impair movement and cause underlying tissue damage.
Causes and Risk Factors
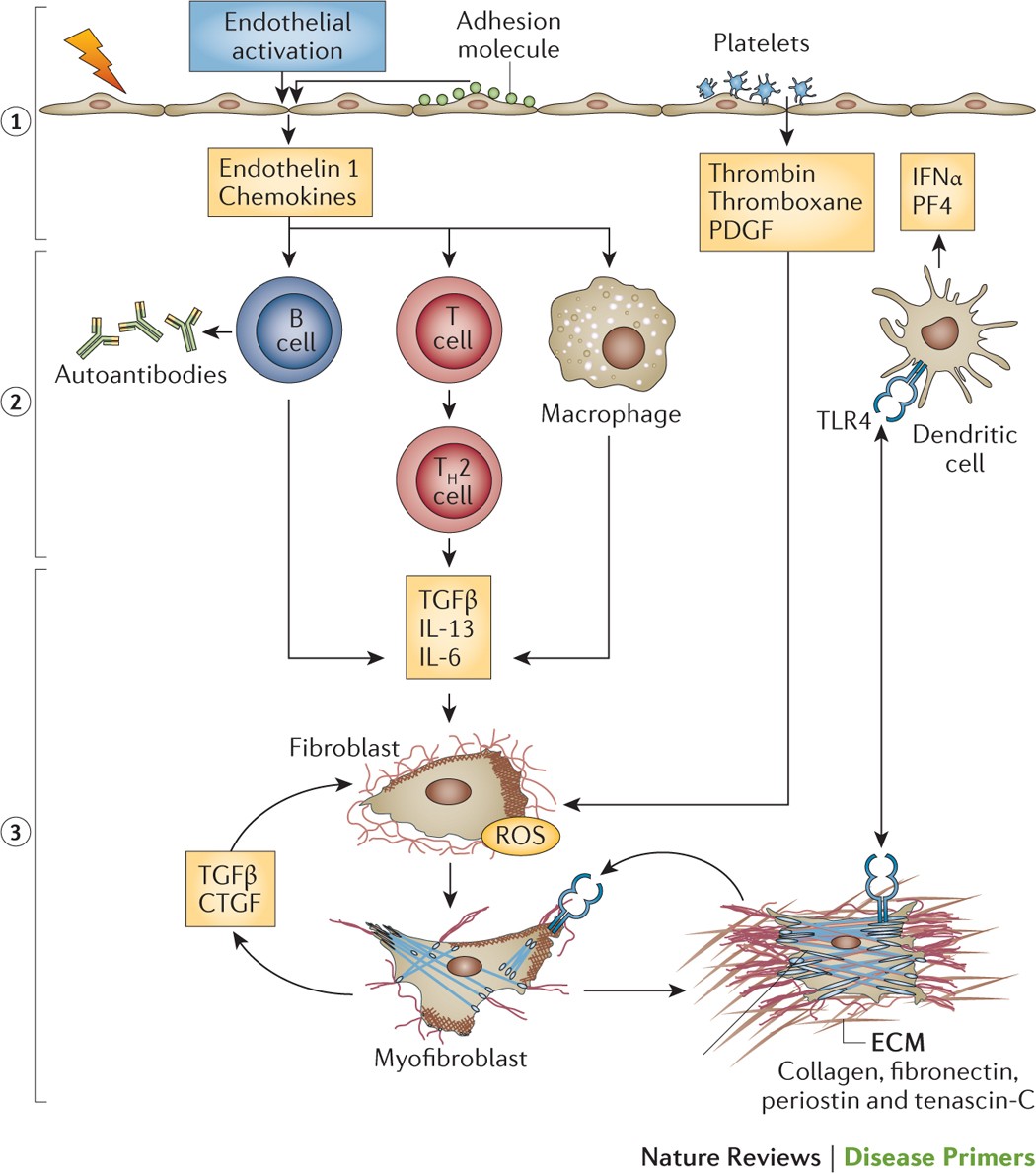
The exact cause of morphia derma is poorly understood, but it is believed to be linked to an abnormal immune response. In this condition, the immune system mistakenly attacks the skin, leading to inflammation, overproduction of collagen, and eventual scarring of the skin tissue. This fibrotic response results in the characteristic hardening of the skin.
Potential Causes Include:
- Genetic Factors:
- Some studies suggest a genetic predisposition, though no single gene is responsible for the condition.
- Environmental Triggers:
- Infections, trauma to the skin, or exposure to certain environmental factors may trigger or exacerbate the condition.
- Autoimmune Response:
- The immune system’s abnormal response may play a key role in the development of morphia.
Risk Factors:
- Age:
- Morphia derma typically affects individuals between the ages of 20 and 50, although it can occur in children as well.
- Gender:
- Women are more likely to develop morphia derma than men.
- Family History:
- Individuals with a family history of scleroderma or autoimmune diseases may be at higher risk.
Symptoms of Morphia Derma
The primary symptoms of morphia derma involve the skin, and they typically develop in stages. The progression of the condition varies from person to person.

Early Symptoms:
- Red or Purple Patches:
- Initially, the affected skin may appear reddish or purple, resembling bruises.
- Swelling and Tenderness:
- The area may be swollen and tender to the touch, though the pain usually subsides over time.
Later Symptoms:
- Thickening of Skin:
- The skin gradually hardens and becomes shiny. This is due to excessive collagen production.
- Loss of Skin Flexibility:
- As the skin becomes thickened and tightened, it loses its ability to stretch, leading to restricted movement.
- Scarring:
- Over time, the hardened areas may develop a scar-like appearance and may become discolored.
- Hyperpigmentation or Hypopigmentation:
- The affected skin may either become darker (hyperpigmentation) or lighter (hypopigmentation) than the surrounding skin.
Other Potential Symptoms:
- In severe cases, morphia derma can affect underlying tissues such as muscles or bones, leading to deformities and joint problems.
- Involvement of the head or face may cause cosmetic concerns, affecting self-esteem and quality of life.
Diagnosing Morphia Derma
Diagnosing morphia derma is primarily based on a patient’s clinical history and the appearance of the skin. A dermatologist typically conducts a physical examination and may perform the following tests:
Skin Biopsy
A biopsy may be performed where a small sample of the affected skin is removed and examined under a microscope. This can confirm the diagnosis and help differentiate morphia derma from other conditions.
Blood Tests
Blood tests can help rule out other autoimmune diseases or infections. Although no specific test exists to diagnose morphia derma, these tests can provide valuable insights.
Imaging Tests
In cases where deeper tissues or bones are involved, imaging tests like X-rays or MRI scans may be recommended to assess the extent of damage.
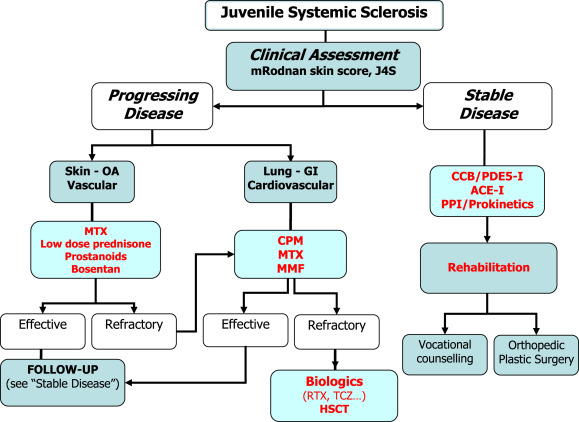
Treatment Options for Morphia Derma
While there is no known cure for morphia derma, treatments aim to manage symptoms, reduce skin thickening, and improve quality of life. The choice of treatment depends on the severity of the condition and the specific form of morphia derma.
Topical Treatments
- Corticosteroid Creams:
- These are often used to reduce inflammation and slow the progression of skin thickening.
- Vitamin D Creams:
- Topical vitamin D analogs can help to manage skin changes.
- Tacrolimus Ointment:
- This immunosuppressive ointment is sometimes used to prevent the immune system from attacking the skin.
Systemic Treatments
For more severe cases, systemic treatments may be necessary:
- Oral Corticosteroids:
- Prednisone may be used to manage inflammation and prevent further thickening of the skin.
- Methotrexate:
- A chemotherapy drug that suppresses the immune system, methotrexate is sometimes used for generalized morphia derma.
- Mycophenolate Mofetil:
- Another immunosuppressive drug is used to reduce inflammation and prevent further tissue damage.
Physical Therapy
For individuals whose skin thickening impairs movement, physical therapy may help maintain joint flexibility and prevent deformities.
Living with Morphia Derma
Living with morphia derma can be challenging, especially if the condition affects cosmetic appearance or physical mobility. However, with early diagnosis and appropriate treatment, many individuals can manage their symptoms effectively. Patients need to maintain regular follow-ups with dermatologists to monitor the progression of the disease and adjust treatment as needed.
Mental Health Considerations
The visible effects of morphia derma, especially on the face or hands, can impact an individual’s self-esteem and mental health. Psychological support, counseling, or support groups may be beneficial in coping with the emotional challenges of living with a chronic skin condition.
Conclusion
Morphia derma, while rare, is a chronic condition that requires ongoing management. By understanding its symptoms, potential causes, diagnostic methods, and treatment options, individuals can seek timely care and improve their quality of life. Though no cure exists, the right combination of therapies can help control the disease’s progression and minimize its impact on daily life. Regular monitoring and support are crucial for individuals living with morphia derma.